<p><br> <span class="small">July 01, 2025</span></p>
How agentic AI is redefining claims processing
<p><b>Agentic AI can autonomously handle exceptions in claims processing, enabling insurers to resolve even edge cases with the speed and confidence once reserved for straightforward claims.</b></p>
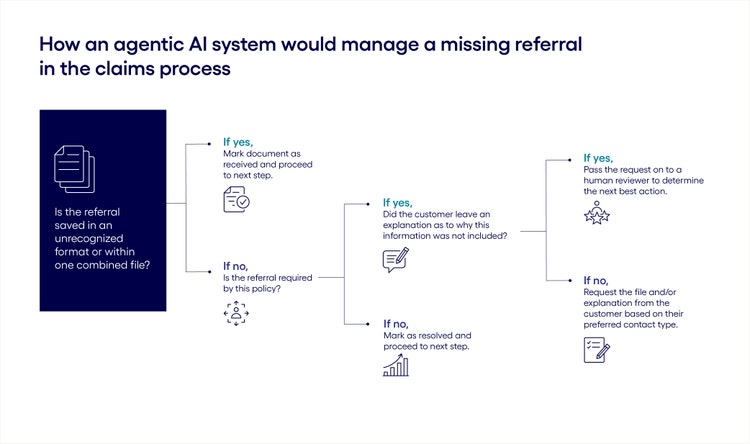
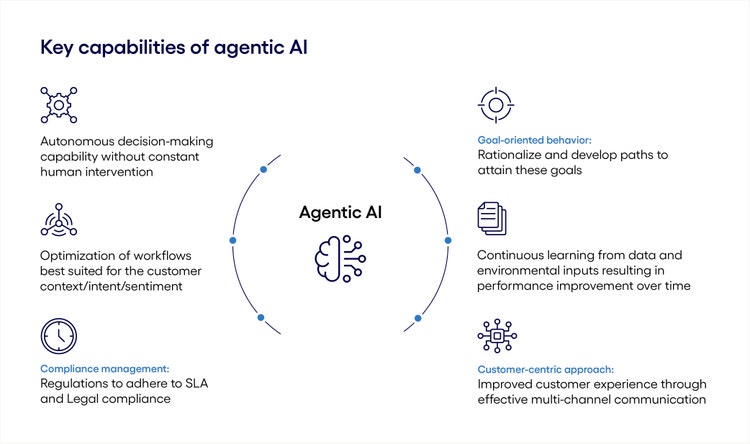
<p>For many insurance companies, the average claim processing time depends on the complexity of the case, the length of the queue and, increasingly, who—or what—is processing it. While standard timelines may take days or weeks, if a customer’s case is being managed by an AI-powered system like <a href="https://www.insurtechinsights.com/lemonade-sets-new-record-by-settling-claim-in-two-seconds/" target="_blank">Lemonade’s AI Jim</a>, a valid claim can be processed in mere seconds.</p> <p>For years, automation and traditional AI tools like AI Jim have played a defining role in the claims process, managing routine tasks like document validation, policy eligibility checks or fraud reviews—routine being the operative word.</p> <p>Unfortunately, when the usual process hits a snag—when a document is missing, a name doesn't match, or a claim is miscategorized or misrouted—delays aren’t measured in seconds but in days or even weeks. This is due to the need for human agents to step in and resolve what the AI system can’t manage.</p> <p>But this may not be the case for long. Agentic AI is introducing a new layer of intelligence through proactive, adaptive learning. Unlike traditional systems that follow a rigid, rule-based approach, agentic AI can learn in real time how to manage common (or not-so-common!) errors, storing the solution and executing it later when the same issue arises—thus making the exception part of the routine.</p> <h4>Enhancing claims processing automation with agentic AI</h4> <p>The two biggest differentiators of agentic AI compared with traditional automation are the ability to continuously learn and then leverage that intelligence to make decisions. In practice, this means that agentic AI can automate many of the routine exceptions that require logic, reasoning and judgment within the claims process.</p> <p>Take, for example, document reviews. Most health insurance claim submissions require the policyholder to submit documentation, such as receipts, physician reports or referrals, to support their claim. Traditional AI has been used to automate the collection and review of those documents based on predefined rules and specific parameters.</p> <p>But so often, this process gets delayed or derailed because submitted documents fall outside the scope of the tool’s intelligence. For example, a file may be missing or saved in an unsupported format—or it may not even be required at all. In these cases, a human must step in to review the error, determine the solution and take the next action.</p> <p>For many companies, the real loss here isn’t just slowing down an individual case, but the need for humans to consistently review and resolve common exceptions across many different cases.</p> <p>With a self-learning, adaptive agentic AI system, companies can reduce or eliminate this need. Unlike traditional AI systems, which have a limited grasp on nuance and low situational awareness, agentic AI can contextualize a task within the broader process. It can recognize patterns and link common errors with approved solutions based on past learnings. And it can execute the resolution according to the roles and capabilities it has been granted.</p> <p>For example, let’s say our health insurance company’s document review tool flagged a missing referral. An agentic solution could manage this situation just as a human would, asking a series of questions to find the next best action:</p>
#
<p><span class="small">Figure 1</span></p> <h4>Five additional use cases for agentic AI in claims processing</h4> <p>The power of agentic AI stretches far beyond document checks. Here we explore five additional ways agentic AI can apply its adaptive learning and intelligence decision-making capabilities to the claims processing lifecycle.</p> <ol> <li><b>Data entry:</b> Agentic AI can process both structured and unstructured data. It can extract information from diverse sources like customer emails, chatbot transcripts, reports and handwritten notes from health providers, technicians and authorities. And because it can contextualize information and infer meaning, it can provide a more accurate and complete view of the case, setting a solid foundation for how the claim should be processed in subsequent steps.<br> <br> </li> <li><b>Claims triage:</b> Agentic systems can also understand the intent behind the claim, as well as the desired business outcome. Because of this, they can autonomously take the next-best action based on the unique circumstances of each case, from flagging the case for a human reviewer, to proactively reaching out to the customer for more information or requesting a fraud review.<br> <br> </li> <li><b>Documentation review:</b> Agentic AI solutions go beyond the static rules that govern a chatbot and continuously learn from real-world cases. For example, when submitting an automotive insurance claim, the policyholder typically needs to submit photos, an estimate for repairs and a police report. But what if, instead of photos, the customer submits a video? Or, instead of a police report, the customer shares body cam footage from the responding officer. The inclusion of these files would derail a traditional AI tool. But with agentic AI, once the solution learns how to recognize, analyze and apply this additional documentation, the exception inspires a new pathway.<br> <br> </li> <li><b>Customer support:</b> Agentic AI can interpret customer intent, tone and emotion in real time, enabling more adaptive, intelligent interactions. For example, if a customer is growing frustrated due to a delayed or potentially denied claim, the AI tool can assess the situation and take proactive steps, such as escalating the issue to a human agent or providing an updated resolution timeline with the customer.<br> <br> </li> <li><b>Fraud detection:</b> Leveraging predictive analytics and pattern recognition, agentic AI can proactively identify irregularities in claims data. By analyzing legal records and historical claims, an agentic AI tool can flag potentially fraudulent claims for further investigation, helping insurers detect and address risk early.<br> <br> For example, an agentic AI system might detect a pattern where a healthcare provider is submitting multiple reimbursement claims for procedures during the same time and dates—which may suggest that some or all of the procedures are fraudulent. An AI tool is likely to recognize this pattern sooner than a team of human reviewers.</li> </ol>
#
<p><span class="small">Figure 2</span></p> <h4>Best practices for successfully applying agentic AI to claims processing</h4> <p>Agentic AI can play a valuable role in enhancing claims processing speed, accuracy, scale and compliance—but only if companies design, implement, integrate and operate effective systems.</p> <p>Here are three recommendations for leveraging agentic AI effectively and getting the most out of the agentic AI investment:</p> <h5><span style="font-weight: normal;"><span class="text-bold-italic">1.</span> Invest in high-quality, real-world training data before deployment</span></h5> <p>The performance and decisioning accuracy of agentic systems are only as strong as the data they are trained on. Training models with simplistic or unrealistic datasets can lead to erroneous outputs, increased customer dissatisfaction and the need for human rework. To fully realize the value of agentic AI in claims processing, organizations must invest in robust, high-quality training data that reflects real-world complexity.</p> <h5><span style="font-weight: normal;"><span class="text-bold-italic">2.</span> Design for data privacy, compliance and auditability from the outset</span></h5> <p>Companies need to address compliance requirements and governance frameworks early in the implementation process to ensure trustworthy, scalable deployment. This means:</p> <ul> <li>Architecting AI systems to operate without the need for accessing sensitive information</li> <li>Excluding protected health information (PHI) and personally identifiable information (PII) from training data sets</li> <li>Establishing regular audits of training data and model outputs to confirm that restricted data has not been used</li> <li>Ensuring the AI system cannot access restricted datasets either directly or indirectly</li> </ul> <h5><span style="font-weight: normal;"><span class="text-bold-italic">3.</span> Train AI systems to recognize when to bring humans in the loop</span></h5> <p>Autonomous AI may be capable of learning on the job to make intelligent decisions, but it should not be empowered to make incorrect decisions due to lack of context or oversight. To ensure fairness and accuracy, AI must be exposed to complex, real-world scenarios during training. This enables the system to learn when and how to make sound decisions and identify edge cases where human judgment is required.</p> <h4>Embracing the role of agentic AI in claims processing</h4> <p>As agentic AI continues to evolve, it promises to shrink the gap between routine processes and exceptions—enabling insurers to resolve even edge cases with the speed and confidence once reserved for straightforward claims.</p> <p><i>For more information on how Cognizant can help you expand the use of agentic AI in your claims management process, read our </i><a href="https://www.pega.com/agentic-ai" target="_blank" rel="noopener noreferrer"><i>complete guide to agentic AI.</i></a></p> <p> </p>
<p>Debjani has over 19 years of experience in MS .NET and Pega BPM technologies. She has successfully led end-to-end project implementations for US and APAC clients in the healthcare, banking & financial services, retail, travel and hospitality domains.</p>


