The proliferation of Digital Health technologies in the life sciences and healthcare industry promises the shift to a patient-centric approach to diagnose, treat, and predict diseases. Imagine a scenario in which a patient can predict when they will need to go to the doctor before a cardio-vascular condition could set in.
With today’s ubiquitous technologies such as smart phones and connected devices such as watches, scales, oximeter etc., patients could make their own health decisions without the need to consult with their doctor. However, until we have a “Digital Health Twin” on our smart phones that could assess our complete health status as well as our family disease histories, there is still a long way to go. The future of Digital Health depends on access to patient data and the seamless interoperability of data on digital systems in the healthcare ecosystem.
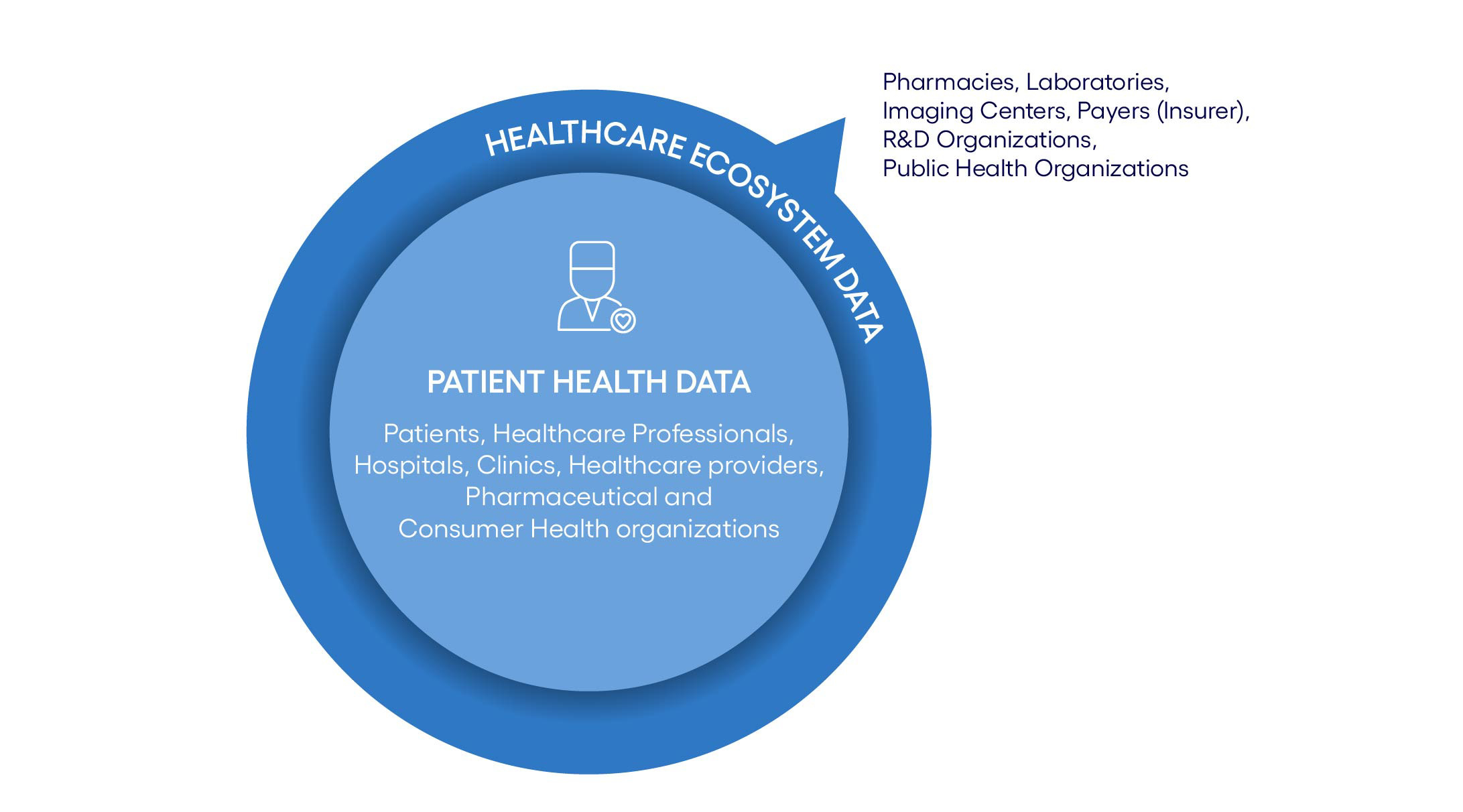
Data in the life sciences and healthcare industry originate from multiple entities (see Figure 1), serving multiple purposes. Patients’ healthcare-related data sets are typically referred to as Patient Health Data. This includes clinical data, prescriptions, electronic health records (EHR), clinical trials data from pharma organizations etc. as well as family records. Such data originate from hospitals, healthcare professionals and pharmaceutical organizations. Digital technologies allow patients to bring in their near real-time data captured using personal devices such as watches, and IoT devices. These real-time data usually reside within different departments of healthcare or consumer health organizations that may not fully exploit their intrinsic value. Patients’ data that reside outside of their primary care unit are called Healthcare Ecosystem Data, and include data from pharmacies, laboratories, imaging centers, R&D organizations, and public health organizations. This cross-organizational data operability is critical to unlocking the data potential in Digital Health. Enabling cross-organizational interoperability of Digital Health data, requires different actors in the healthcare ecosystem to mutually share data.