<p><br> <span class="small">August 08, 2025</span></p>
Healthcare spotlight: The One Big Beautiful Bill Act
<p><b>We explain strategic priorities for healthcare payers as the new legislation begins to impact the industry—and the nation.</b></p>
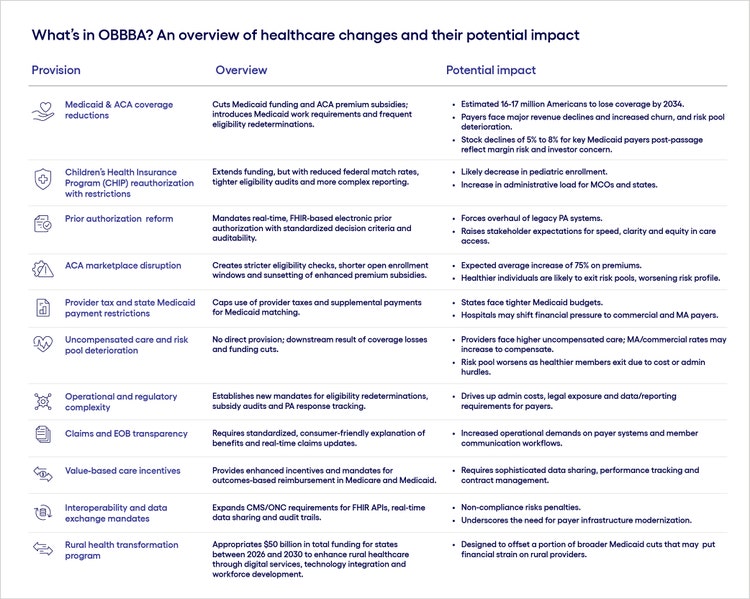
<p>The One Big Beautiful Bill Act (OBBBA) is now law—ushering in sweeping healthcare-related changes as part of the latest federal budget reform.</p> <p>For healthcare organizations, this legislation represents more than just a compliance challenge; it’s a crossroads. Leaders must decide whether to react narrowly to meet the specific demands of the moment or use this disruption as a catalyst for broader, lasting transformation.</p> <p>Here we’ll break down key provisions of the bill and analyze their impact on healthcare operations and industry dynamics. We’ll also share five best practices to help healthcare organizations move from reactive compliance to proactive resilience, positioning themselves to weather future disruptions with confidence and agility.</p>
#
<p><span class="small">Figure 1</span></p> <h4>Facing change with confidence: 5 key strategic priorities for payers</h4> <p>Regulatory change is just one of many disruptive forces driving healthcare organizations to evolve. As companies adapt to meet the new needs of OBBBA, they should consider not just the requirements of the law but how strategic investments can help insulate the company from future market evolutions.</p> <p>Here are steps companies can take to move away from siloed, reactive approaches toward holistic, technology-driven strategies that foster flexibility, scalability and long-term resilience.</p> <h5><span class="text-bold-italic">1</span>. Drive member retention and satisfaction through enhanced experiences</h5> <p>While OBBBA’s direct impact has yet to be revealed, most analysts agree it will increase membership churn, especially for managed care organizations (MCOs). Stricter eligibility checks, shorter open enrollment windows and sunsetting of enhanced premium subsidies within the Affordable Care Act (ACA) may also limit new enrollments in health plans and health exchanges.</p> <p>In this context, the membership experience becomes even more critical, as retention and satisfaction are the keys to stable, sustainable growth.</p> <p>For example, Elevance Health (formerly Anthem) launched <a href="https://www.elevancehealth.com/our-approach-to-health/consumer-centered-health-system/sydney-health-app-simplifies-healthcare" target="_blank" rel="noopener noreferrer">Sydney Health</a>, an all-in-one mobile app that simplifies key parts of the care journey, such as finding providers, getting care and managing prescriptions. Rather than using technology to drive operational efficiencies, Elevance leaned into human-centered design to help members better understand and use their benefits. And it worked: The company reported that on any given day in 2024, about half of members had used the app in the previous 90 days.</p>
<p><span style="font-weight: 400;"><br> For example, to increase care consistency, Aetna Medicaid, CVS Health, the National Alliance for Care at Home and MissionCare Collective launched </span><a href="https://apc01.safelinks.protection.outlook.com/?url=https%3A%2F%2Fwww.cvshealth.com%2Fnews%2Fmedicaid%2Faetna-national-alliance-for-care-at-home-and-missioncare-collective-unite-to-strengthen-direct-care-workforce.html\&data=05%7C02%7CNathan.Conz%40cognizant.com%7Cd496e95fe744484147f608ddd01405ad%7Cde08c40719b9427d9fe8edf254300ca7%7C0%7C0%7C638895506749689769%7CUnknown%7CTWFpbGZsb3d8eyJFbXB0eU1hcGkiOnRydWUsIlYiOiIwLjAuMDAwMCIsIlAiOiJXaW4zMiIsIkFOIjoiTWFpbCIsIldUIjoyfQ%3D%3D%7C0%7C%7C%7C\&sdata=zOfUj59%2FRG6ZTRS8ohse4sWVugQVpYEuY8pRNhvHmV0%3D\&reserved=0" target="_blank" rel="noopener noreferrer">a program to improve home health worker retention</a><span style="font-weight: 400;">. As part of the program, designated providers in Illinois, Louisiana and North Carolina are rolling out </span><a href="https://apc01.safelinks.protection.outlook.com/?url=https%3A%2F%2Fwww.coachupcare.com%2F\&data=05%7C02%7CNathan.Conz%40cognizant.com%7Cd496e95fe744484147f608ddd01405ad%7Cde08c40719b9427d9fe8edf254300ca7%7C0%7C0%7C638895506749707557%7CUnknown%7CTWFpbGZsb3d8eyJFbXB0eU1hcGkiOnRydWUsIlYiOiIwLjAuMDAwMCIsIlAiOiJXaW4zMiIsIkFOIjoiTWFpbCIsIldUIjoyfQ%3D%3D%7C0%7C%7C%7C\&sdata=Kt0zTSEBSQIUinTH8mUYTAXB2sZt3qv6xjdLHhAzkQQ%3D\&reserved=0" target="_blank" rel="noopener noreferrer">CoachUp Care</a><span style="font-weight: 400;">, a data-powered workforce tool to better support health workers in their day-to-day interactions and equip leaders with actionable insights to prevent turnover.</span></p> <h5><span class="text-bold-italic">2</span>. Optimize costs through advancing technology, new operating models and strategic divestments</h5> <p>OBBBA heightens the urgency surrounding greater efficiency, as Medicaid and ACA coverage reductions—along with new provider taxes and state Medicaid payment limits—are expected to reduce enrollments. At the same time, new reauthorization requirements and stricter eligibility checks will add to payers’ administrative burden.</p> <p>Technology has long played a role in the healthcare cost efficiency equation, but the growing use of intelligent solutions, including generative and agentic AI, are enabling even greater improvements. For example, Omega Healthcare implemented <a href="https://www.businessinsider.com/omega-healthcare-uipath-ai-document-processing-health-transactions-2025-6?utm\_source=chatgpt.com" target="_blank" rel="noopener noreferrer">AI-powered billing and claims automation</a>, resulting in 15,000 employee hours saved per month, a 40% reduction in documentation time, and a 50% improvement in turnaround times.</p> <p>AI and analytics can also help address the new law’s key provision around prior authorizations. The legislation, which mandates real-time, FHIR-based electronic prior authorization with standardized decision criteria and auditability, will force an overhaul of legacy prior authorization (PA) systems. However, with the use of AI tools, healthcare organizations could significantly reduce, or even eliminate, the need for prior authorizations by giving payers real-time, data-driven insight into a patient’s status.</p>
<p><br> For example, in organizations with high cloud maturity, it may also be possible to explore operational consolidation strategies—such as leveraging global capability centers or offshore models—to outsource administrative and back-office functions, freeing up local resources to focus on higher-value priorities.</p> <p>Organizations can also use the introduction of OBBBA to reevaluate their portfolio. Leaders should assess their geographic footprint, doubling down on profitable regions while considering consolidation or divestment in underperforming areas.</p> <h5><b><span class="text-bold-italic">3</span>. </b>Enhance data sharing and performance tracking to capitalize on new value-based care model incentives</h5> <p>OBBBA supports the transition to outcomes-based reimbursement in Medicare and Medicaid, pushing providers toward value-based care and alternative payment models that prioritize care management and cost containment to maximize reimbursement in a restrictive payment landscape.</p> <p>While this shift will be seen as a potential bright spot by some, it also underscores the need for sophisticated data sharing, performance tracking and contract management. For payers, the goal is no longer just building a large provider network but fostering a highly effective one—where connectivity, transparency and coordinated interventions drive measurable results.</p> <p>For example, <a href="https://business.optum.com/en/insights/tech-vbc-models-enhancing-payer-provider-partnerships.html?utm\_source=chatgpt.com" target="_blank" rel="noopener noreferrer">Optum One</a> enables near-real-time, bidirectional sharing of claims and clinical data. This empowers providers to close care gaps faster and personalize interventions, driving better outcomes at lower costs for both parties.</p> <p>To develop these capabilities, organizations may be able to leverage the <a href="https://www.kff.org/medicaid/issue-brief/a-closer-look-at-the-50-billion-rural-health-fund-in-the-new-reconciliation-law/" target="_blank" rel="noopener noreferrer">Rural Health Transformation Program</a>, a $50 billion fund included in OBBBA, to support value-based care transformation in underserved areas. However, states must apply by the CMS-designated deadline to access funding opportunities related to care delivery redesign, data infrastructure and workforce development.</p> <h5><b><span class="text-bold-italic">4</span>. </b>Broaden the definition of care to include health and wellness</h5> <p>The new legislation creates an opportunity, and a need, for payers to rethink how they approach wellness—an area in which many have traditionally struggled.</p> <p>This is particularly true for vulnerable Medicaid populations. Many of those expected to be most affected by OBBBA face higher rates of chronic and behavioral health conditions, which require proactive care and ongoing management. At the same time, many of those people also deal with social determinants like poor nutrition and housing insecurity, which makes it harder to engage them in established wellness programs.</p> <p>This underscores the need for companies to not only view health more holistically but take an innovative and thoughtful approach to wellness program design.</p> <p>For example, SCAN Health Plan, a non-profit Medicare Advantage plan and healthcare services provider based in California, partnered with Instacart to develop a <a href="https://www.scanhealthplan.com/about-SCAN/press-release-archive/SCAN-2025-Medicare-Advantage-Offerings-Focus-on-Lower-Costs-Expanded-Benefits" target="_blank" rel="noopener noreferrer">grocery allowance</a>. The program helps seniors access “nutritious, culturally tailored food options” that support their overall wellbeing and also help them manage chronic conditions, such as diabetes and cardiovascular disease.</p> <p><a href="https://www.careoregon.org/members" target="_blank" rel="noopener noreferrer">CareOregon</a>, a non-profit health insurer focused on serving low-income individuals through the Oregon Health Plan (that is, Medicaid), offers gift cards and other incentives for members who engage in preventative services like well-child visits, immunizations and dental check-ups or chronic condition management programs. For some members, CareOregon also offers benefits to address broader health influencers, such as housing, nutrition and extreme weather.</p> <h5><b><span class="text-bold-italic">5</span>. </b> Embrace analytics, AI and platform modernization across the transformation strategy</h5> <p>OBBBA has highlighted the need for healthcare organizations to transform to meet the needs of the new market. This includes both offering new health services, plans and tools to boost growth; and leveraging new models and systems to reduce costs. The one thing both sides of the equation have in common is the need for a strong digital core that helps the organization modernize and optimize.</p>
<p><br> For example, as noted above, AI can be used to streamline the burdensome PA process—a key focus of recent legislation. By accelerating and even automating this process, AI can reduce administrative delays, ease friction for providers and patients, and improve overall care delivery. The same can be said of claims adjudication.</p> <h4>Meeting the law while seizing the larger opportunity</h4> <p>As the 2025 budget reform ushers in sweeping changes, healthcare organizations face a critical choice: react narrowly to the demands of new legislation or seize this moment to drive broader, lasting transformation.</p> <p>While compliance is essential, the real opportunity lies in modernizing operations, adopting flexible technologies and building the resilience needed to navigate not just today’s policy shifts, but the constant evolution of the healthcare landscape.<br> </p>
<p>Raj Ramaswamy is an Assistant Vice President, leading the payer strategy & Industry Solution Group within Cognizant’s healthcare business. In this capacity, Raj directs Cognizant’s strategic direction, healthcare offerings, and M&A initiatives, while driving the advancement of innovative health technology solutions. He’s also responsible for developing partnership ecosystems and fostering cross-industry collaborations</p>
<p>Heather Hodges is a seasoned healthcare professional with over 15 years of experience across payer, provider, and consulting sectors. She currently focuses on driving transformative initiatives at the intersection of policy, technology, and population health. Heather is passionate about health equity, data-driven reform, and challenging the status quo in the US healthcare.</p>



